Post date:
New insights on the use of flexible manufacturing to support the response to emergencies such as the COVID-19 pandemic have just been published by an academic-NHS-industry partnership in which the School of Engineering played a leading role.
COVID-19 caused crippling global supply shortages of medical equipment and materials. At an early stage of the pandemic, the University of Edinburgh, NHS Lothian and several companies (AESSIS, Lomond Process Engineering, GemDT and Shapespace) came together as a team to address this problem by reverse engineering or redesigning critical hardware for healthcare applications.
In a paper published on Monday 2 August in a special issue of Frontiers in Medical Technology, the 26-person consortium – which includes students, postdoctoral researchers, technicians and academics from the School of Engineering – present the lessons learned from their work.
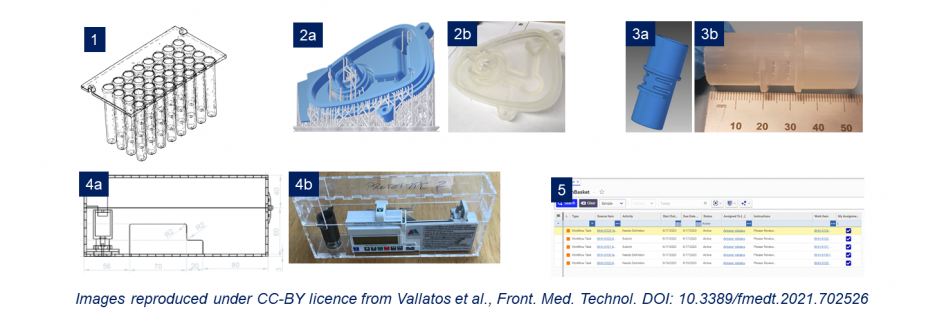
Some members of the team used high-tech three-dimensional scanning methods to study existing biomedical hardware and endeavoured to make replacements using 3D-printing.
Others set out to design and build a new lock-box that could be used to securely hold syringe pumps, which are used to deliver medication such as painkillers.
A third group within the consortium focused on a software solution that could be used to manage the development of bespoke healthcare hardware products, such as equipment to help directly with patient care or parts that are needed to keep important machines in operation.
The group’s findings demonstrate that flexible manufacturing has the potential to secure back-up supply chains for future emergencies, using pop-up ‘nanofactories’ that can adapt rapidly to developing situations. Their experience shows that such ‘adaptive’ manufacturing must be data-driven and will need to blend old-fashioned engineering techniques with new cutting-edge methods.
The team’s paper also discusses the numerous technical and legal complexities involved in the development of customised components for use in clinical medicine.
The University team included members drawn from the School of Engineering, the College of Medicine and Veterinary Medicine, the School of Informatics and the uCreate Studio.
The project was led by Dr Katherine Dunn of the School of Engineering, who said: "The team worked very hard on a wide range of projects, bringing together expertise from academia, industry and the NHS. We hope that our work will be instructive to others endeavouring to develop flexible manufacturing for emergency situations, in the context of clinical engineering or elsewhere."
Read the paper: Adaptive Manufacturing for Healthcare During the COVID-19 Emergency and Beyond.